Could the “Sunshine Vitamin” help in the fight against COVID-19?
The Sunshine Vitamin and COVID-19
Scientists have been looking for volunteers to take part in a new study to investigate the impacts of vitamin D, the 'sunshine vitamin', on the immune system. The study aims to determine whether taking vitamin D can help to increase immunity against respiratory diseases, including COVID-19, as some studies suggest a correlation between people with lower vitamin D levels and more severe COVID-19 symptoms.
Please note that this article is not intended as medical advice!
The trail, known as CORONVIT, is run by researchers from the Queen Mary University of London. David Jolliffe, principle investigator believes that the trial “has the potential to give a definitive answer” to the question of whether vitamin D can offer protection against COVID-19. The trial will run for six months and involves 5,000 participants who will be required to undergo a test to indicate whether an individual has a vitamin D deficiency. If so, participants will be sent vitamin D supplements. Scientists will then measure if participants experience any doctor-diagnosed or laboratory-confirmed acute respiratory infection over the six-month trial. The aim of this is to determine if vitamin D can help in protecting people from COVID-19.
An estimated one billion people worldwide have vitamin D deficiencies. The deficiency is mainly caused by lifestyle factors such as reduced outdoor activities as well as environmental factors such as air pollution, and other factors that reduce exposure to sunlight. Factors such as gender, living at a higher latitude, and greater amounts of physical activity levels are also associated with differences in vitamin D levels. The National Health Service (NHS) recommends that the general population should consider taking vitamin D supplements, as 40% of the UK’s adult population have inadequate levels of vitamin D over the winter and spring months.
How vitamin D was discovered: (Norval, 2005)
- The mid-1600s – Whistler and Glisson, independently published a scientific description of rickets (a bone deformity caused by a deficiency of vitamin D). However, they could not identify a cure for the disease.
- The 1840s – A Polish physician called Sniadecki observed that children living within the industrial centre of Warsaw were more likely to have rickets, whereas children living in the countryside were less likely to develop the disease. The observation led him to theorise that the lack of exposure to sunlight was the cause of the disease.
- 1918 – Sir Edward Mellanby tested the difference diet made to rickets on beagles. He found that beagles that were housed indoors and fed a diet of only oatmeal were more likely to develop rickets. However, beagles that were given cod liver oil in their diets, were cured of the rickets disease.
- At the time it was unknown to Sir Mellanby what elements of the cod liver oil helped cure the beagles of rickets. It was later found that cod liver oil contained Vitamin D, a fat-soluble vitamin
- The 1920s and 1930s – Windus et al. uncovered the various chemical structures of the different forms of vitamin D.
- 1936 – A biologically active form of vitamin D named D3 was detected in skin. D3 forms as a result of the reaction between ultraviolet radiation and 7-dehydrocholesterol. As such, vitamin D was characterised as a steroid. Very soon after this discovery, it was found that the components in cod liver oil that cured rickets were vitamin D3, to be exact.
Different forms of Vitamin D and its structure:
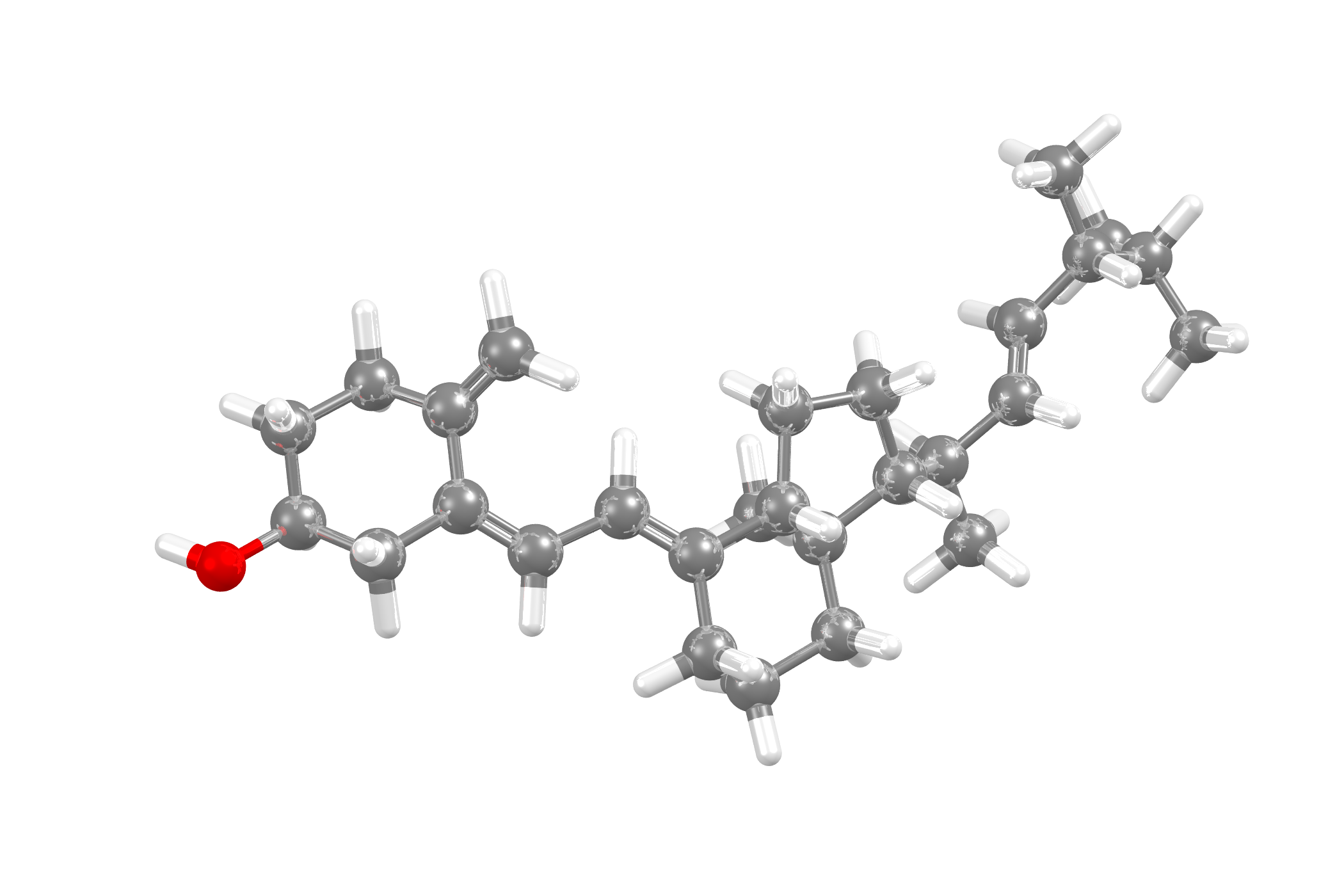
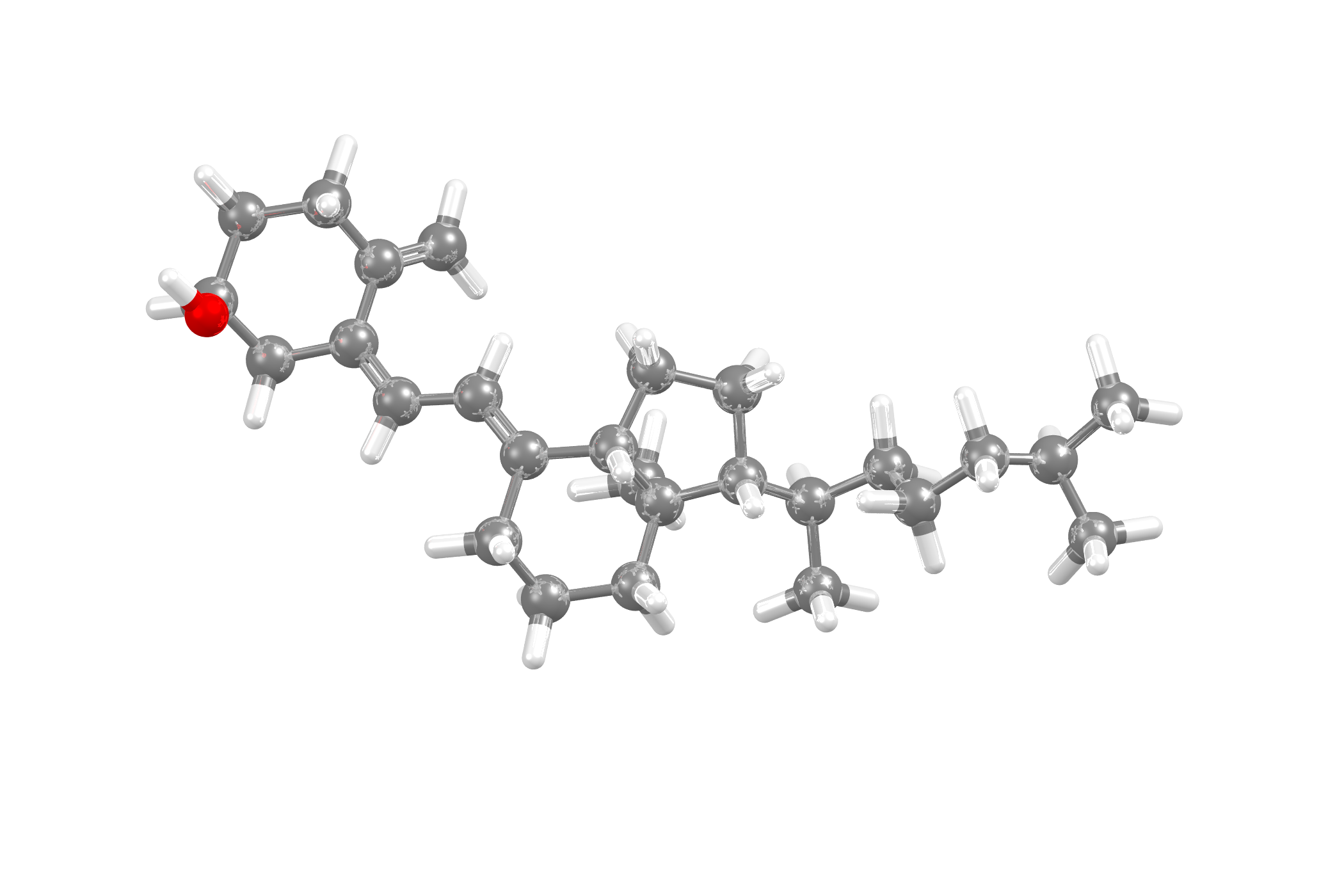
Vitamin D belongs to a family of lipids called secosteroids. Secosteroids share very similar structures to steroids, the difference being that two of the carbon atoms on the second ring are not joined, as they would be in a regular steroid. Vitamin D is affected by a complex network of feedback mechanisms involving multiple enzymes and receptors, which indicates that it reacts more like a steroid than a nutrient.
Vitamin D has two major forms, vitamin D2 (ergocalciferol) and vitamin D3 (cholecalciferol). Vitamin D2 is largely human-made and added to foods. Vitamin D3 is synthesized in the skin of humans from 7-dehydrocholesterol and is also consumed via animal-based foods.
The structural difference between vitamin D2 and vitamin D3 is in the side chain. Vitamin D2 contains a double bond between carbons 22 and 23, and also has a methyl group on carbon 24. These differences do not affect the metabolism and both forms function as prohormones. When both vitamin D2 and D3 react in the body they exhibit identical responses.
Vitamin D2The CSD shows four recorded structures of vitamin D2 |
Vitamin D3The CSD shows four recorded structures of vitamin D3 |
 |
 |
Why we need vitamin D and how it reacts:
Vitamin D that is obtained from sun exposure, foods, and supplements is biologically inert. Vitamin D and its metabolites are carried around the body in the blood, bound to the vitamin D binding protein (DBP) and albumin. Both vitamin D2 and D3 are absorbed in the small intestine. The vitamin then goes through two different hydroxylations in the body to activate. The first hydroxylation occurs in the liver, where vitamin D is converted to 25-hydroxyvitamin D [25(OH)D], or more commonly known as “calcidiol”. The second hydroxylation happens primarily in the kidneys and produces the physiologically active 1,25-dihydroxy vitamin D [1,25(OH)2D], also known as “calcitriol”.
Vitamin D is needed to regulate calcium and phosphorous minerals in our bodies, and it is also important to enable normal bone mineralisation. It also helps to prevent hypocalcaemia tetany (involuntary contraction of the muscles, which cause cramps and spasms). Without vitamin D, bones can become thin, brittle, or misshapen and can also cause rickets in children and osteomalacia in adults. Vitamin D also reduced the amount of inflammation in the body, as well as, regulating cell growth, neuromuscular and immune function, and glucose metabolism.
What is next?
The trials to understand the effects of taking vitamin D supplements to prevent major COVID-19 symptoms are still in the developmental stages. It would be interesting to see if taking the supplements helps to build some immunity to the virus. Spain is also now looking into how vitamin D levels are drastically low in COVID-19 patients and researching how vitamin D could be useful against COVID-19.
However, it is important to note that the study is still ongoing and there is no indication on whether vitamin D can help fight COVID-19, therefore, everyone should continue following government guidelines.
See our other blogs on COVID-19 to learn about the research CCDC are working on in this area, and how you can get involved.
Tags